Break the cycle - How probiotics and prebiotics can provide relief from IBS
Irritable Bowel Syndrome (IBS) remains one of the most common gastrointestinal disorders, affecting approximately 10% of the population.* It is characterised by a complex combination of causes, triggers and symptoms. IBS can significantly impact the quality of life of those affected and symptoms can last for days, weeks, or even months.
This blog aims to understand IBS, offering insights into its nature, causes, types, and various management strategies to help those affected navigate the condition more effectively.
What is IBS?
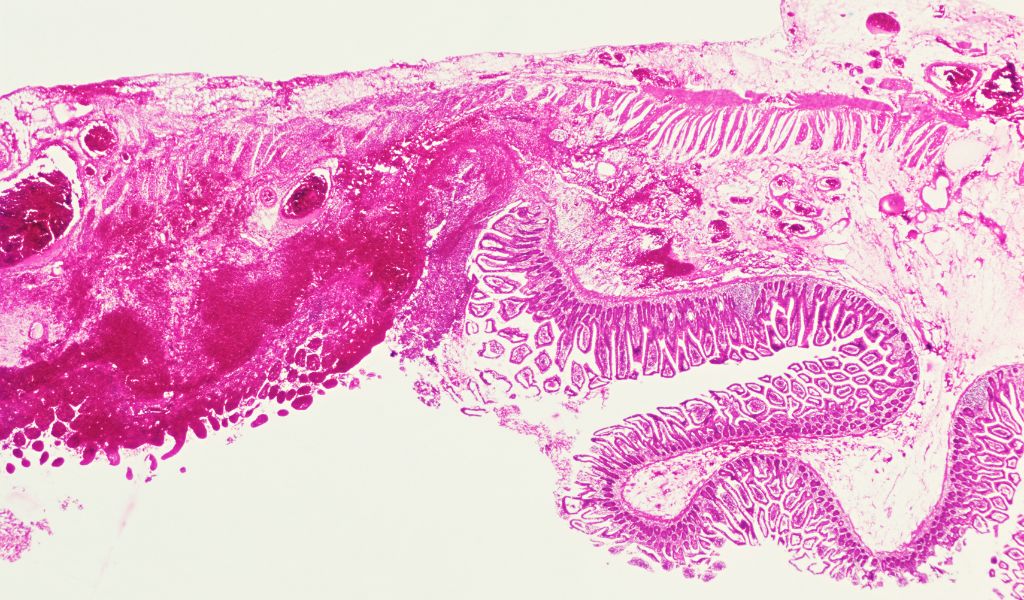
Irritable Bowel Syndrome (IBS) is a gastrointestinal disorder characterised by a group of symptoms that typically occur together. These include recurrent abdominal pain and changes in bowel habits such as diarrhoea, constipation, or a combination of both. IBS is a chronic condition that requires long-term management.
IBS vs IBD: The difference between irritable bowel syndrome (IBS) and irritable bowel disorder (IBD)
IBS and IBD are two conditions that affect the digestive system and are often confused due to their similar names and symptoms. Both are chronic conditions that cause abdominal pain, cramping, and urgent bowel movements. However, despite having similar acronyms and symptoms, these two conditions are very different in their nature, causes, and how they're treated. Here's a breakdown of the key differences:
| Irritable Bowel Syndrome (IBS) | Irritable Bowel Disease (IBD) |
| Classified as a syndrome, defined as a group of symptoms. | Classified as a disease. |
| Related to problems with how the gut works. It doesn't cause visible damage to tissues. | Often used to describe two chronic conditions: Crohn's disease and ulcerative colitis. These are autoimmune diseases are characterised by chronic inflammation of the gastrointestinal tract and can cause permanent harm to the intestines. |
| There is no sign of disease or abnormality during an exam of the colon. Diagnosis is usually made based on symptoms and after ruling out other conditions. | Diagnosis is made through a combination of tests, including blood tests, stool tests, endoscopy, and imaging studies to look for inflammation and damage. |
| Treatment focuses on symptom management and may include dietary changes (like following a low FODMAP diet), stress management, and medications to relieve specific symptoms. | Treatment aims to reduce inflammation, control symptoms, and maintain remission. This can include the use of anti-inflammatory drugs, immune system suppressors, and sometimes surgery. |
IBS is a functional disorder without visible damage to the digestive tract, primarily managed through symptom control and lifestyle changes. IBD, on the other hand, involves chronic inflammation and can cause significant damage to the GI tract, requiring more specific and sometimes aggressive treatment to manage inflammation and prevent complications.
Symptoms of IBS

The symptoms of IBS vary between individuals and affect some people more severely than others. Symptoms can become worse, often during times of stress or after eating certain foods.
Some of the symptoms of IBS ease after going to the toilet:
- Stomach pain and cramping
- Change in your bowel habits – such as diarrhoea, constipation or sometimes both
- Bloating
- Excessive wind
- Occasionally experiencing an urgent need to move your bowels
- Fatigue
- Nausea
- Heartburn
- Back pain
What causes IBS?
Although the exact cause of IBS remains unclear, it is believed to be a result of multiple factors, including alterations in gut motility and food passing through the gut too quickly or slowly, hypersensitivity in the gut and abnormalities in the gut microbiome. Psychological factors such as stress and anxiety can also play a significant role in exacerbating the symptoms.
Often, IBS is referred to as a disorder of the gut-brain interaction and has to do with problems with how our gut and brain coordinate to help our digestive system work. The butterflies you experience in your stomach when you’re nervous or the sinking feeling when you get anxious highlights the strong connection between our emotions, thoughts, and digestion.
Common triggers of IBS

Identifying and avoiding triggers is a key strategy in managing IBS. Common triggers include:
- Dietary factors: Certain foods and drinks can exacerbate symptoms.
- Stress: High-stress levels are known to trigger flare-ups.
- Hormonal changes: Many individuals report a worsening of symptoms during menstrual periods, perimenopause and menopause.
Different types of IBS
IBS is classified into three main types, based on the predominant bowel habit.
- IBS with constipation (IBS-C)
- IBS with diarrhoea (IBS-D)
- IBS with mixed bowel habits (IBS-M)
Understanding the type of IBS is crucial for tailoring treatment effectively.
How is IBS diagnosed?
There is no specific test for IBS. Diagnosis typically involves a process of elimination to rule out other causes of the symptoms. After ruling out other conditions through tests such as blood tests, stool tests, and colonoscopy, IBS is diagnosed if no other cause is found.
How long does IBS last?
IBS is a chronic condition, meaning symptoms can last for years or even a lifetime. However, symptoms can change over time and many people can manage their symptoms effectively with treatment and lifestyle adjustments.
Who is at risk for IBS?
Those more likely to be at risk for IBS are:
• Younger people: most people first get IBS before they are 45 years old.
• Women: women get IBS almost twice as often as men.
• Have had recent gastroenteritis.
Link between IBS and menopause
Hormonal fluctuations during menopause can affect gastrointestinal function, potentially exacerbating IBS symptoms. Some women report the onset or worsening of IBS symptoms during this period.
Treatment for IBS
Treatment is typically multifaceted, including:
Medications: Different medicines are used for IBS, depending on the symptoms. These include medicines to prevent constipation, diarrhoea, pain, and spasms.
Psychological Therapies: Stress management strategies like cognitive behavioural therapy (CBT) can be effective.
Dietary Adjustments: Tailoring the diet to minimise consuming foods that trigger symptoms. In some cases, a high-fiber diet can reduce symptoms.
Probiotics: To help restore and balance the gut microbiome.
Regular exercise: Helps to reduce stress and can promote bowel function.
Adequate sleep: Essential for overall health and stress management.

What is a FODMAP diet?
Diet plays a crucial role in managing IBS. FODMAP is an acronym that stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. These are small carbohydrates that are difficult to digest and can be fermentable by bacteria in the gut, leading to increased gas, bloating, and other IBS symptoms.
A low FODMAP diet involves reducing the intake of these carbohydrates and is effective for many people with IBS.
Examples of FODMAPs:
- Oligosaccharides: garlic, onions, legumes, and wheat.
- Disaccharides: mainly sucrose, lactose (mostly in dairy products), and maltose.
- Monosaccharides: simple sugars such as fructose and glucose found in fruit, honey, and sugary drinks.
- Polyols: found in stone fruits, many sugar-free sweeteners, and some vegetables like mushrooms.
Food high in FODMAPs:
| Fruits | Grains | Vegetables | Legumes |
| Apples | Barley | Artichoke | Almonds |
| Apricots | Couscous | Asparagus | Baked Beans |
| Blackberries | Rye | Beets | Black Beans |
| Cherries | Semolina | Brussels Sprouts | Black-Eyed Peas |
| Figs | Wheat | Butternut Squash | Broad Beans |
| Mango | Cauliflower | Cashews | |
| Nectarines | Fennel | Chickpeas | |
| Peaches | Garlic | Kidney Beans | |
| Pears | Leeks | Lentils | |
| Plums | Mushrooms | Pinto Beans | |
| Prunes | Onions | Pistachios | |
| Pomegranates | Soybeans | ||
| Split Peas |
Food low in FODMAPs:
| Fruits | Grains | Vegetables | Nuts & Seeds |
| Banana | Brown Rice | Aubergine | Almonds |
| Grapes | Buckwheat | Bean Sprouts | Brazil Nuts |
| Kiwi | Maize | Bok Choy | Chia Seeds |
| Lemon | Millet | Cabbage | Hazelnuts |
| Limes | Oats | Carrot | Macadamia Nuts |
| Oranges | Polenta | Choy Sum | Peanuts |
| Papaya | Quinoa | Cucumber | Pecan |
| PassionFruit | Tapioca | Green Bell | Pine Nuts |
| Pineapple | Pepper | Pumpkin Seeds | |
| Rhubarb | Kale | Sesame Seeds | |
| Strawberry | Lettuce | Walnuts | |
| Okra | |||
| Tomato | |||
| Spinach | |||
| Yam |
Probiotics & the gut microbiome
The gut microbiome is the name for the trillions of microbes that live in our gut. Research has shown that the health of our gut microbiome has a profound impact on our overall health and holds a connection with our brain, skin and immune system. It is therefore no surprise that the gut microbiome plays an important role in IBS.
Probiotics are live microorganisms, often referred to as "good" or "friendly" bacteria. They are found in fermented foods like yogurt, kefir, and supplements. Many factors can cause an imbalance of the healthy bacteria in the gut such as antibiotics, stress, illness, and lifestyle. When an imbalance occurs, known as dysbiosis, gastrointestinal disorders such as IBS can occur.
Therefore, by re-balancing the gut microbiome with probiotics, you can help restore the balance of intestinal flora, improving gut motility, immune function, and immune response.
The NHS recommends that probiotics can be used to help manage the symptoms of IBS and that they should be continued for at least 4 weeks.
Several strains of probiotics have been studied for IBS, with some showing promise in alleviating symptoms such as bloating, gas, and abdominal pain. Commonly researched strains include Lactobacillus, Bifidobacterium, and Saccharomyces boulardii.
Prebiotics
Prebiotics primarily serve as food for the friendly gut bacteria, helping to nourish and allow them to thrive. This, in turn, helps to improve the overall health of the gut microbiome, which we know is closely linked with digestive and gut health.
As highlighted above, IBS has a broad range of symptoms. It is important to look for supplements containing probiotic strains that have been found to offer benefits for IBS. Look for a high-quality daily supplement for all-round gut support.
What makes a good probiotic supplement?
We know that the market is saturated with hundreds of different probiotics and it can often be a minefield to navigate. Here’s what to look for to ensure you are choosing the best probiotic for you:
- Multi strain: different probiotic strains have different effects on health. Some strains can be beneficial for general gut health, while others are specifically targeted for conditions like IBS and immune health. Looking for supplements that have included a variety of strains will have the biggest positive impact on your gut health.
- CFU count: CFU stands for colony-forming units, which indicate the number of live and viable microorganisms in a probiotic. While higher CFU counts are often thought to be more effective, the optimal count depends on the specific strain and the health condition being targeted. Some conditions might benefit from a higher CFU count, while for general maintenance, a lower count might be sufficient.
- Prebiotics: prebiotics, are fibres that feed the beneficial bacteria in your gut. This combination, often referred to as a symbiotic, can enhance the probiotic's effectiveness.
- Delivery to the gut: probiotics are very delicate and easily damaged by stomach acid. It is important to ensure the probiotic you are taking reaches the gut where it is most beneficial.
- Stability: some probiotics need to be refrigerated to maintain their potency, while others are shelf-stable due to special formulations or packaging. Always check the label for storage instructions.
- Purity: look for supplements that do not contain unnecessary additives and bulking agents that may negatively impact your symptoms. Some probiotics may even contain dairy, soy, gluten, or other common allergens.
Gut Love
Gut Love is our pre and probiotic supplement designed to help restore the balance of healthy bacteria within the gut.
It contains 19 strains of healthy bacteria and 2 strains of prebiotics providing 19 billion CFU per two capsules.
One of the prebiotics in the formulation, slippery elm, also provides stability to the formulation and ensures delivery of the probiotics to the gut. It creates an emulsion barrier around the probiotics ensuring they reach the gut safely.
Gut Love does not need to be refrigerated and should be stored in a cool, dry location away from direct sunlight.
It is dairy and gluten-free and free from any other synthetic additives and ingredients.
Gut Love is an effective treatment choice for individuals suffering with IBS. It will help to restore the balance of healthy bacteria in the gut and reduce symptoms such as bloating, cramps, and irregular bowel habits as well as strengthen your immune system.
Understanding and managing IBS requires a comprehensive approach, involving dietary and lifestyle adjustments, stress management, and sometimes medication. Each individual’s experience with IBS is unique, and finding what works best for you might take time and experimentation.
Call our Pharmacists if you have concerns
Our expert pharmacists are always on hand to answer any questions you might have and to make tailored recommendations based on your individual needs. Please contact us for free health advice on:
@: pharmacist@thenakedpharmacy.com
T: 01483 685 630
Dimple Varu

Dimple is a pharmacist with 12 years of experience working in retail and general practice and now specialises in providing education and advice on natural supplements.
She believes in the power of nature and using natural existing compounds to enhance our health, whether that’s treating pain or helping to prevent long-term conditions. Mum of 1, living a busy life, loves reading and baking if she has the time.